|
Histopathological
findings in hysterectomy specimens:
A retrospective study
......................................................................................................................................................................
Suad Mohamed O. Zaid (1)
Mazen Abood Ben Thabet (2)
(1) Department of Morphololgy Sciences, Faculty
of Medicine, University of Aden
(2) Department of Paraclinic, Faculty of Medicine,
University of Aden
Correspondence:
Suad Mohamed O. Zaid
Department of Morphololgy Sciences,
Faculty of Medicine,
University of Aden
Email: salamomer54@yahoo.com
|
ABSTRACT
This is a retrospective study of descriptive
patterns of findings seen in hysterectomy
specimens based on records from a Modern
- histopathology laboratory in Aden.
A total of 2,544 specimens were analyzed
during the 6 years period from January 2006
to December 2012, to study the histopathological
findings of these specimens. The age of
the patients at hysterectomy ranged from
16-80 years with a mean of 44.6, with the
maximum patients (56.3 %) in the age group
41-50 years and less patients in less than
30 years.
Most common pathology findings are; Endometrial
hyperplasia 1481 (58.3%), Non neoplastic
cystic lesion 1386 (54.5%), Chronic cervicitis
1363 (53.6%), Adenomyosis 793 (31.2% ) follow
by Leiomyoma 697 (27.4%).
Other less frequent pathologies identified
included atrophic endometrium, Inadequate
secretory endometrial transformation,
Gestational Trophoblastic disease, Endometroid
adenocarcinoma, cervical prolapse.
This study confirms that benign pathologies
are more common in hysterectomy specimens
than their malignant counterparts.
Key words: Hysterectomy,
endometrial hyperplasia, ovarian cystic
lesion, chronic cervicitis.
|
Uterus,
a vital reproductive organ is subjected to many
benign and malignant diseases. Many treatment
options are available including medical and conservative
surgical but hysterectomy still remains the most
common gynaecological procedure performed worldwide
(1).
The procedure is not well embraced
in developing countries, thus, the clinical indication
for the procedure should be justifiable, for age
and parity of the women (2).
In response to the consistent
demand for this procedure, hysterectomy has been
identified as a key health care indicator in recent
reports, to measure and compare hospital performance
(3).
It is the definitive cure for
many of its indications which include dysfunctional
uterine bleeding, fibroids, utero-vaginal prolapse,
endometriosis and adenomyosis, pelvic inflammatory
disease, pelvic pain, gynaecological cancers and
obstetric complications. Ultimate diagnosis is
only on histology, so every hysterectomy specimen
should be subjected to histopathological examination
(4).
In Yemen, histopathological examination
of hysterectomy specimens carries diagnostic and
therapeutic significance. Prevalence of uterine
and adnexal pathologies varies from nation to
nation and from region to region (5)
The present study is aimed at
detailed histopathological evaluation of all lesions
of hysterectomy specimens. It provides an intact
uterus and consequent control over tissue sampling
and hence enabling determination of origin of
particular lesion and to compare the findings
with other researchers.
Our study
was a retrospective descriptive work analysis
of 2,544 patients with hysterectomy, over a period
of 6 years from January 2006 to December 2012.
The information was gathered regarding age, and
histological diagnosis and was analyzed by Excel
program and tables performed according to the
objectives of the study and compared to literature
review.
A total
of 2,544 hysterectomy specimens between January
2006 to December 2012 were analyzed. The age range
of the patients was 16 to 80 years, with a mean
of 47.6 years.
Of these 2,544 cases, most of
the cases were in the 41-50 years age group 1431(56.3%),
which is the most common age group for contracting
various diseases as shown in Table 1.
Table 1: Distribution of patients according to
age groups
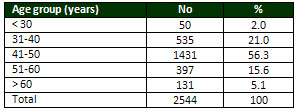
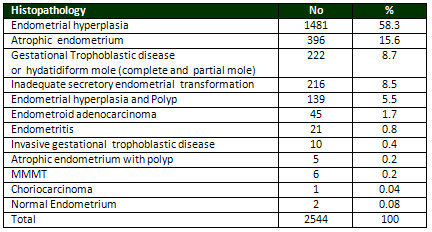
Table 2 revealed that out of
the total hysterectomy specimens 1,481(58.3%)
were Endometrial hyperplasia, atrophied endometrium
396 (15.6%) Tumor was present in specimens out
of which 10 were invasive complete hydatidiform
mole, 45 were endometrial adenocarcinomas , Malignant
mixed mullerian tumour (MMMT) 6 (0.2%) cases and
one case of choriocarcinoma.
Table 2: Histopathological findings in Endometrium
hysterectomy specimens
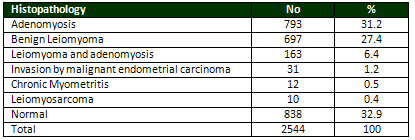
Most common histopathological
abnormality in myometrium was adenomyosis followed
by Leiomyoma. Adenomyosis in 793 (31.2%), followed
by Isolated leiomyoma was seen in myometrium of
697 (27.4%) hysterectomies, where in 163 (6.3%)
myometriums, both were present together. Tumor
was present in specimens out of which 31 was invasive
by malignant endometrial carcinoma as shown in
Table 3.
Table 3: Histopathological findings in myometrium
In Table 4 cervix from 2,377
(53.6%) specimens showed chronic cervicitis. Cervical
intraepithelial neoplasia (CIN) I, CIN II, CIN
III with chronic cervicitis (0.8%, 0.4, 0.3%)
and flat condyloma (0.1%,0.6%), squamous cell
carcinoma were seen in 22 specimens (0.9%) and
Adenocarcinoma were 17 cases. Uterovaginal prolapse
were 132 cases (5.2%).
Table 4: Histopathology of cervix
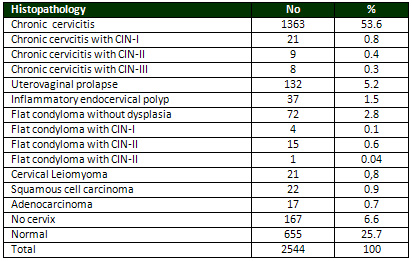
Unremarkable Histopathology of
the cervix were 655 cases (25.7%).
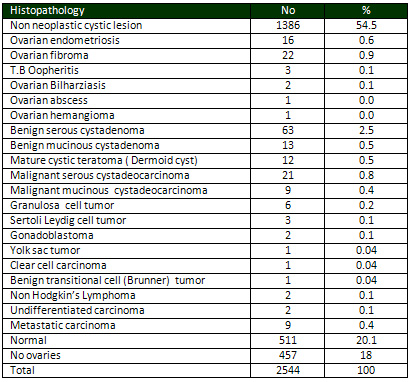
2,087 ovarian specimens were
retrieved from the computerized database of the
pathology department, from January 2006 to December
2013.
There were 1,386 (54.4%) non-neoplastic
functional cysts.
The neoplastic were benign serous
cystadenoma (2.5 %) and benign varian fibroma
(0.9%), mucous cystadenoma (0.5%) and Mature cystic
teratoma (Dermoid cyst) 0.5%.
The malignant were 21 cases of
serous cystadeocarcinoma , 9 cases of mucinous
cystadeocarcinoma , 2 cases undifferentiated carcinoma
and 9 cases of Metastatic carcinoma, as appears
in Table 5.
Table 5: Histopathology of
ovaries
Hysterectomy is the commonest
gynecological operation and the rate of hysterectomy
varies according to geographic
distribution, patient and physician related factors
(1).
Hysterectomy is second only to
cesarean section as the most frequently performed
major operation in the United States. Approximately
600,000 hysterectomies are performed annually
in the USA, and more than one third of US women
have had a hysterectomy by the age of 60 (6).
In Pakistan, the rate of hysterectomy
is quite high because it is the only surgical
option available if the patient is not responding
to medical treatment(7).
Many women in Africa and Nigeria
in particular are reluctant to undergo this procedure
because of the socio-cultural attachment to procreation
and taboos associated with lack of menstruation(2).
Few studies have been performed
describing the pathologic findings in hysterectomy
specimen and examining the relationship between
the preoperative clinical indication and pathologic
diagnosis (8).
In the present study, the mean
age of patients was 47.6 years and age range from
16 to 80 years which was nearly similar to findings
by others (7,9,10).
The peak age for the procedure
in our study was the fourth decade (41–50
years) as has been observed in other studies (9).
In the current work we found
endometrial hyperplasia was the commonest histopathological
finding with 58.3%.
Lee (11) reported that endometrial
hyperplasia was confirmed in 95%, a somewhat higher
figure than we found and less results 16% were
found in Nepal by Ranabhat et al (5).
Endometrial hyperplasia is
either idiopathic or occurs due to associated diseases
or conditions. It can also be transformed to endometrial
carcinoma and patients with endometrial hyperplasia
must be treated properly and carefully followed
up (12).
The exact pathogenesis of endometrial
polyps is not fully elucidated, but they are thought
to originate as a localized hyperplasia of the
basalis, perhaps secondary to hormonal influences
(13).
In our study the association
between endometrial hyperplasia and hyperplastic
endometrial polyp were 139 (5.5%) cases.
This figure approaches that seen
by Kelly et al (14) with (3.1%) in all cases of
endometrial hyperplasia in his study period. Other
studies have found that incidence of endometrial
polyps in endometrial hyperplasia range between
11 and 29% (15).
In the present study we found
atrophic changes in 396 cases (15.6%), nearly
approximate to that seen by Ranabhat et al (5)
with 13% and that seen by Pity et al (16) from
Iraq with 10.4 %.
A higher figure was seen in study
by Thamilselvi et al (17) with 26%.
This may justify the sample size in our study.
Other authors were in discordance
with our study, Gousia et al (18) reported 5.44%,
and results reported by Sarawathi et al (19) with
2.44%.
In the present study inadequate
secretory transformation were 216 (8.5%) cases,
which was similar to other findings (20).
It is higher than that seen by
Zeeba et al (21) with 1.8% and higher than our
result was reported by Sarfraz et al (22) with
24%.
Chronic endometritis is commonly
seen in the reproductive age due to either retained
products of conception, pelvic inflammatory diseases
or other pregnancy related conditions.
In our study 21 (0.8%) cases
showed chronic endometritis of all hysterectomy
samples, which approximate with the finding of
Sajjad et al (23) which was 1% and completely
lower than that seen by Ranabhat et al (5) which
was 9.5%.
We found in our study endometrial
adenocarcinoma were in 45 patients (1.7%). This
finding is similar to that found by others (5,16),
but it was completely lower than those reported
by Patel (24) from Australia 10.5%, and by Gebauer
et al (25) from Germany with 16%.
Gestational Trophoblastic
Disease (GTD) refers to a wide spectrum of interrelated
conditions ranging from benign hydatidiform mole
(HM), invasive mole to malignant choriocarcinoma
(26).
These regional variations have
been reported with many speculative factors such
as ethnic origin, blood group, age, parity, diet
and nutrition, contraception, socio-economic status,
immunologic factors and genetic constitution (27).
In our study we found 222 (8.7%)
cases of GTD of the total hysterectomies samples,
only 10 cases were invasive gestational trophoblastic
disease at the time of pathological diagnosis
and one case of choriocarcinoma.
In the Kingdom of Saudi Arabia
(KSA) fifty-nine cases of hydatidiform mole, 36
complete hydatidiform mole (CHM) and 23 partial
hydatidiform mole (PHM) and 2 cases of choriocarcinoma
were observed, out of 64,762 pregnancies registered
at Security Forces Hospital, Riyadh, KSA, during
an 11 year period (27).
In a study in Nepal, there were
17 (37.8%) cases of hydatidiform mole, 6 (13.3%)
of invasive mole and 22 (48.8%) patients of choriocarcinoma
(28).
A malignant mixed Mullerian tumour
(MMMT) of the uterine corpus is an extremely rare
and aggressive malignancy, comprising only 1–2%
of uterine neoplasms (29).
In our study there were 6 (0.2%)
cases of MMMT. In the study of Rajshekar SK only
four cases of MMMT were diagnosed representing
20% of his sample (30) and this variation in the
frequencies may support our justification related
to sample size and study design.
In the current study adenomyosis
was the commonest lesion of the myometrial pathology
and represented 31.1% followed by leiomyoma 27.4%.
Adenomyosis appears also to be the commonest pathology
and similar to our findings reported by others
(5,22,31).
The present study revealed that
leiomyoma was also the commonest pathology and
it was 27.4%. Reported frequencies vary in different
countries and it was 26% in KSA (32), and 36%
and in Kurdistan/Iraq (16), in Nigeria 48%(33)
and 17% in India (34) and only 8% in Sweden (35).
Some of the hysterectomy specimens
show more than one lesion in the body of uterus,
of which coexistence of adenomyosis and leiomyoma
are the most common (34).
In the present study there was
6.4% showing coexistence of adenomyosis and leiomyoma.
In other study increasing to 56% when adenomyosis
with concomitant leiomyoma are included (31) and
it was 19% reported by Sarfraz et al (21) and
5.6% reported by Qamar et al (7).
Leiomyoma was the commonest lesion
of uterine corpus followed by adenomyosis.
This was similar to findings of other studies
(16,32,33,36,37).
Geographical and racial influences
are thus apparent on the prevalence of uterine
leiomyoma and the prevalence of risk factors in
terms of quantities and type. Early menarche,
delayed menopause, decreased parity, obesity and
lack of exercise are some of the risk factors
of leiomyoma (5).
Among the cervix uteri, chronic
cervicitis was the main pathological finding in
the present study and accounted for 53.6%. This
figure is nearly similar to that reported by Jamal
et al (36) which was 41.5% and to that reported
by Qamar et al (7) which was 31%.
A higher figure of chronic cervicitis
seen in Nepal women by Jha et al was 96.4% (37);
the variation may be related to different reproductive
health procedures. Iin Yemen almost all males
are circumcised which minimizes vaginal infection.
In our study 37 (1.5%) cases
showed dysplasia of various degrees with chronic
cervicitis and 20 (0.7%) cases showed cervical
condyloma with dysplasia.
A premalignant lesion, Cervical
intraepithelial neoplasia (CIN) was seen in 3.0%
in a study by Thamilselvi et al (17) and 0.8 %
reported by Ranabhat et al (5).
The low incidence of CIN in our
study may related to the reproductive life style,
where the women are restricted to single sexual
partner , while the CIN is more common with sexually
transmitted disease of HPV, which is more frequent
in multiple sexual partner women .
The diagnosis of uterovaginal
prolapse was based on clinical as well as pathological
findings (38).
In our study Hysterectomies done
for utero-vaginal prolapse were found in 132 (5.2%).
This finding was higher than that reported by
Pity et al (16) which was 2(0.5%), while less
than the findings reported by Butt et al (39)
with (11%) and less than 17% reported by Adelusola
et al (33).
The present study revealed only
0.9% of all the samples of hysterectomy showing
invasive squamous cell carcinoma at the pathological
study.
This finding was nearly similar
to that reported by Ranabhat et al (5), Gousia
RR et al (18) and Bani et al (40) which were 0.6%,
0.3% and 0.6% respectively.
This low incidence may be related
to reproductive health in Arab and Muslim countries
where most of the women are restricted to one
sexual partner and a Muslim habit for washing
and vaginal douches after sexual intercourse and
a high incidence of HPV infection in European
countries play an important role in cervical dysplasia
and carcinoma.
In the present study adenocarcinoma
were 17 (0.7%) cases.
Garud et al in 1981 described
adenocarcinoma of cervix also carries considerable
percentage i.e. 15-20% of all invasive carcinoma
of cervix (41), while Sanyal et al (42) noted it
as 2% among all cervical lesions.
The most common lesions encountered
in the ovary include functional or benign cysts
and tumors and benign ovarian neoplasms occur
at any age whereas malignant ovarian neoplasms
are more common in the elderly (43,10).
Ovarian tumors are one of the
major causes of gynaecological problems in females
and present with marked variation in their histological
types. Relative frequency of these lesions is
different for Western and Asian countries (10).
We found in our current study,
the most common pathological finding of the ovaries
in all hysterectomy samples were benign (functional)
cysts and were 54.4%.
Our finding was nearly similar
to that reported by Mansour (44) in KSA where
the benign non neoplastic ovarian cysts comprise
47.5%, while the data from South East Asia shows
that 90.5% of ovarian cysts were benign (45),
less results were reported by Gupta et al (46)with
2.77% and 20% by Ranabhat et al (5).
Surface epithelial tumours were
the major histological type of ovarian tumours
followed by germ cell tumours as the commonest
ovarian cyst seen in most of the literature (8).
In our study, the most common
surface epithelial tumors was benign serous cyst
adenoma 2.5% followed by mucinous cystadenoma
0.5% , which approximate the finding seen by Jha
et al (37) with 4.5% for benign serous cystadenoma,
3.1% for mucinous cystadenoma and 25.7% of benign
surface epithelial tumors were serous cyst adenoma
and 6.7 % were mucinous cyst adenoma reported
by Pity et al (16) in their study, which was lower
than that seen by Abdullah et al (38) where serous
cystadenoma represented 44.6% and mucinous cystadenoma
13.6%. The low figure in our study may be related
to the study sample, where we are selected only
hysterectomy samples and excludes all cases with
simple ovarian cystectomies.
In our study malignant serous
cystadenocarcinoma were the most common malignant
ovarian neoplasm and represented 0.8% of the cases
followed by mucinous cystadeocarcinoma 0.4% and
this figure approximates the data published by
Jha et al (37) where 3.4% of his cases are malignant
serous cystadenoma and 0.8% were malignant mucinous
cystadenoma.
The higher result with data published
by the others, and it’s 33.3% for malignant
serous cystadenocarcinoma and 15.4% for malignant
mucinous cystadenocarcinoma seen by Abdullah et
al (38) and in Nepal malignant serous cystadenocarcinoma
account for 21.1% and 22.2% of malignant mucinous
cystadenocarcinoma found by Jha et al (37) and
the low figure in our study related to the type
of study sample.
Approximately 95.0% of ovarian germ cell tumors
are mature cystic teratomas in the western world
(47).
In this study mature cystic teratoma
(Dermoid cysts) account for 12 (0.5 %) of all
ovarian tumors. A study in Pakistan (48) reported
a high figure of 38%.
A mature cystic teratoma is a
benign neoplastic ovarian lesion that occurs during
reproductive life and is more common in young
females during active reproductive life and usually
treated by simple cystectomy and this may justify
the low incidence in our study where the hysterectomy
is the sample study and not ovarian cystectomy.
Other ovarian tumours are rare
in our study and it was 0.6% for ovarian fibroma
which is similar to that reported by Jha et al
(37) with 0.9%.
Granulose cell tumor was 6(0.2%)
in our study and it is similar to other findings
(37,49).
In the present study ovarian
endometriosis accounted for 16 (0.6%), which was
similar to that seen by Gousia et al (17) with
(0.61%). Also, our finding was less than that
observed by Randabhat et al (5) which was 8.9%
and less than that seen by Ahsan et al (30) with
13%.
Ovarian endometriosis is a benign
condition usually treated by simple ovariectomies,
which justify the low figure in our study which
is based on hysterectomy samples.
In the present study metastatic
carcinoma to ovaries (secondary) accounted for
9(0.4%) which was lower than that seen by Abdullah
et al (38) with 13(15.5%) and 4(2.4%) reported
by Jha et al (10).
The low figure in our study does
not reflect the low incidence in our patients
but may be related to big sample size in our study
(2,450 cases) as well as the type of sample study
and most cases of metastatic carcinoma to ovaries
are with advanced stages of either breast or GIT
cancer, where there is no indication orfor hysterectomies.
Hysterectomy still remains the
widely used treatment modality even in developed
countries. The ultimate diagnosis
is only on histology, so every hysterectomy specimen
should be subjected to histopathological examination.
Histopathological analysis correlates well with
the pre-operative clinical diagnosis for hysterectomy.
Most of the pathologies
are still benign; malignancies are also detected
on hysterectomy specimens, but very rarely. A
yearly audit should be conducted in every institute
to collect data and to analyze the pattern of
indications and types of histopathological lesions
and pattern of diseases.
1. Vessey MP, Villard-Mackintosh
L, McPherson K, CoulterA, Yeats D. (1992). The
epidemiology of hysterectomy: findings in a large
cohort study. Br J Obstet Gynecol.; 99: 402-7.
2. Ezem BU and Otubu JA. (1981) . Hysterectomy
in the Hausa/Fulani population in Nigeria. Int
J Gynecol Obstet;19:145-9.
3. Toma A, Hopman WM, Gorwill RH. ( 2004 ). Hysterectomy
at a Canadian tertiary care facility: results
of a one year retrospective review. BMC Women
Health.:4(1):10
4. Nausheen F, Iqbal J, Bhatti FA, Khan AT, Sheikh
S. Hysterectomy. (2004). The patient’s perspective.
Annal Gynecol; 10: 339-41
5. Ranabhat SK, Shrestha R, Tiwari M, Sinha DP,
Subedee LR. (2010) . A retrospective histopathological
study of hysterectomy with or without salpingoophorectomy
specimens. JCMC Journal of Chitwan Medical College;
Vol. 1 (1): 24-29
6. Schaffer JI, Word A. (2002 ). Hysterectomy-still
a useful operation. The New England Journal of
Medicine; 347 (17): 1360-1362.
7. Qamar-ur-Nisa, Habibullah, Shaikh TA, Hemlata,
Memon F, Memon Z. (2011). Hysterectomies; an audit
at Tertiary Care Hospital. Professional Med J
Mar;18(1):45-
8. Ahmed M, Malik TM, Afzal S, Mubarik A. (2004).
Clinicopathological study of 762 ovarian neoplasms
at Army Medical College Rawalpindi. Pak J Pathol;15(4):147-152.
9. Carlson KJ. Outcomes of hysterectomy. (1997).
Clin Obstet Gymaecol;40:939-46.
10. Jha R, Karki S. (2008). Histological pattern
of ovarian tumors and their age distribution.
Nepal Med Coll J; 10: 81-85.
11. Lee NC. (1984). Confirmation of pre-operative
diagnosis for hysterectomies. American Journal
of Obstetrics & Gynaecology; 150 (3): 283-7.
12. Caspi E, Perpinial S, Reif A. (1977). Incidence
of malignancy in Jewish women with postmenopausal
bleeding. Israel Journal of Medical Sciences,
13(3):299–304.
13. McGurgan P, Taylor LJ, Duffy SR, O’Donovan
PJ. (2006) Are endometrial polyps from pre-menopausal
women similar to post-menopausal women? An immunohistochemical
comparison of endometrial polyps from pre- and
post-menopausal women. Maturitas ;54:277–84
14. Kelly P, Dobbs S, McCluggage W. (2007). Endometrial
hyperplasia involving endometrial polyps: report
of a series and discussion of the significance
in an endometrial biopsy specimen. BJOG;114:944–950.
15. Bakour S, Khan S, Gupta JK. (2000) . The risk
of premalignant and malignant pathology in endometrial
polyps. Acta Obstet Gynecol Scand;79:317–20.
16. Pity IS, Jalal A. Jalal JA, Hassawi BA . (2011)
. Hysterectomy: A Clinicopathologic Study . Tikrit
Medical J 16 journal; 17(2): 7-16.
17. Thamilselvi R, Sinha P, Subramanium. (2011).
Correlation between clinicopathological and ultrasonographical
findings in hysterectomy. Journal of Clinical
Diagnostic Research;vol.5(4):737-740.
18. Gousia RR, Yudhvir G, Subash B . (2013). Patterns
of Lesions in Hysterectomy Specimens: A Prospective
Study. JK Science. Vol. 15 No. 2.
19. Saraswathi D, Thank Johnson, Shalinee R, Rathi
Rajkumar, Jaya Vijayaraghavan, Vinod Kumar Panicker.
(2011). Study of Endometrial Pathology in Abnormal
Uterine Bleeding. J Obstet Gynaecol India;61(4):426
- 430
20. Talat Mirza1, Saadia Akram, Aamir Mirza1,
Sadiya Aziz, Tariq Mirzaand Tazeen Mustansar .
(2012 ). Histopathological Pattern of Abnormal
Uterine Bleeding. Journal of Basic & Applied
Sciences, Vol. 8, No. 1. Pg 114-117.
21. Zeeba S. Jairajpuri, S. Rana and S. Jetley.
(2013). Atypical uterine bleeding-Histopathological
audit of endometrium. A study of 638 cases. Al
Ameen J Med Sc i; 6 (1) :21-28.
22. Sarfraz R, Ahmed MM, Tariq M. Tahir And M.
Sarfraz Ahmed. (2011). Benign Lesions In Abdominal
Hysterectomies In Women Presenting With Menorrhagia.
Biomedica Vol. 27 .
23. Sajjad M, Iltaf S, Qayyum S. (2011). Pathological
findings in Hysterectomy specimens of patients
presenting with menorrhagia in different age groups.
Ann Pak Inst Med Sci;7:160-2.
24. Patel SRP. (1967) . Postmenopausal bleeding.
MJA. 27:1080-82.
25. Gebauer G, Hafner A, Siebzehnrubl E,Lang N.
(2001). Role of hysteroscopy in detection and
extraction of endometrial polyps: results of a
prospective study. Am J Obstet Gynaecol; 184:59-63
26. Mochizuki M, Maruo T, Matsuo H, Samoto T,
Ishihara N. (1998). Biology of human trophoblast.
Int J Gynecol Obstet; 60: 21-28.
27. Tariq Y. Khashoggi, MCPS, ABOG .(2003). Prevalence
of gestational trophoblastic Disease. A single
institution experience. Saudi Med J; Vol. 24 (12):
1329-1333
28. Pariyar J. (2009). Gestational trophoblastic
disease in Nepalese women managed in B. P. Koirala
Memorial Cancer Hospit. J Clin Oncol (Meeting
Abstracts) vol. 27 no. 15S e16570
29. El-Nashar SA and Mariani A . (2011). Uterine
carcinosarcoma Clin Obstet Gynecol 54(2) 292–304.
30. Rajshekar SK, Guruprasad B, Shakunthala PN,
Praveen Rathod, Uma Devi and UD Bafna. (2013).
Malignant mixed Mullerian tumour of the uterus.
Ecancermedicalscience.; 7: 302.
31. Ahsan S, Naeem S, Ahsan A. (2001). A case
note analysis of hysterectomies. performed for
non-neoplastic indication. Liaquat National Hospital,
Karachi. J Pak Med Ass; 51(10):346-9.
32. Sobande AA, Eskander M, Archibong EI, Damole
IO. (2005). Elective hysterectomy: a clinicopathological
review from Abha Catchment Area of Saudi Arabia.
West Afr J Med24 (1): 31-35
33. Adelusola KA, Ogunniyi SO. (2001). Hysterectomies
in Nigerians: histopathological analysis of cases
seen in Ile-Ife . Niger Post grad Med J. ; 8(1):
37-40.
34. Talukder SI, Haque MA, Huq MH, Alam MO, Roushan
A, Noor Z . (2007). Histopathological analysis
of hysterectomy specimens, Mymensingh J; 16: 18-
24.
35. Borgfeldt C, Andolf E. ( 2000).Transvaginal
ultrasonographic findings in the uterus and the
endometrium: Low prevalence of leiomyoma in a
random sample of women age 25-40. Acta Obstet
Gynecol Scand;79:202-7.
36. Jamal S and Baqai S. (2001). A clinicohistopathological
analysis of 260 Hysterectomies Pakistan. J Pathol.;
12(2): 11-4.
37. Jha R, Pant AD, Jha A, Adhikari RC, Syami
G. (2006).The histopathological analysis of hysterectomy
specimens. J Nepal Med Assoc; 45(163):283-290
38. Abdullah LS, Bondagji NS. (2011). Histopathological
Pattern of Endometrial Sampling Performed for
Abnormal Uterine Bleeding. Bahrain Medical Bulletin,;33(4):1-6.
39. Butt JL, Jeffery ST, Van der Spuy ZM. (2012).
An audit of indications and complications associated
with elective hysterectomy at a public service
hospital in South Africa. Int J Gynecol Obstet.;116
(2):112-116.
40. Bani-Irshaid and Al-Sumadi A. (2011). Histological
findings in women with postmenopausal bleeding:
Jordanian figures.EMHJ . Vol. 17 No. 7.
41. Garud M, Lulla M,Patel K,Saraiya U, Mehataji
S. (1981). Cervical borderline lesions. Ind Obstet
Gynecol Ind:31:135.
42. Sanyal B, Pant GC, Sahni K, Koteshwar Rao
K, Gupta S (1992). Non –epidermoid tumours
of -uterine cervix. J . Obstete Gynecol Ind;32-591
43. Kumar, Vinay; Abbas, Abul K.; Fausto, Nelson;
& Mitchell, Richard N. (2007) . Robbins Basic
Pathology (8th ed.). Saunders Elsevier. pp. 718–721.
44. Mansour I. (2002 ). Ovarian diseases at King
Abdul-Aziz University Hospital. Saudi Med J; 23:
1551-1552
45. Kayastha S. (2009). Study of ovarian tumors
in Nepal Medical College Teaching Hospital. NepalMed
Coll J;11:200-2.
46. Gupta G, Kotasthane D, Kotasthane V. (2009).
Hysterectomy: A Clinico-Pathological Correlation
Of 500 Cases. The Internet Journal of Gynecology
and Obstetrics. Volume 14 Number 1.
47. Tavassoli FA, Devilee P (2003) .WHO Classification
of Tumors. Pathology and Genetics, Tumors of Breast
and Female Genital Organs. IARC Press; 35-36
48. Saeed M. Khawaja K. Rizwan 1, et al. (1991).
Clinicopathological analysis of ovarian tumours.
J. Pak. Med. Assoc.; 41: 161-64.
49. Schumer ST, Cannistra SA. (2003). Granulosa
cell tumor of the ovary. J Clin Oncol; 21: 1180-1189.
|