|
Adaptive Support
Control Volume (ASV) and Early weaning of Ventilator
in Intensive Care Unit
......................................................................................................................................................................
Qasim Khamaiseh
Correspondence:
Dr. Qasim Khamaiseh
Consultant in anaesthesia and intensive care.
Royal Medical Services
Mobile: 00962799018838
Email: qasimkhamaiseh@yahoo.com
|
ABSTRACT
Aim: To
demonstrate the role of choosing the mode
of ventilator in the patient's outcome and
therefore early weaning from ventilators.
Method: After obtaining
the acceptance of our ethical committee
this study was done.
One hundred and twenty six patients were
randomly taken in this study, in two groups;
sixty four patients in group (A) using the
synchronized intermittent mandatory volume
(SIMV), and the other sixty two patients
(B) group using an adaptive control volume
(ASV) as another mode.
Result: We found
that patients who were on adaptive support
volume (ASV) group (B) had faster process
of weaning and early extubation, and showed
better arterial blood gases with easier
management, which lead to early discharge
from the ICU.
Conclusion: Training
to use the new mechanical ventilators modes
like adaptive support ventilation (ASV)
is advisable, in some patients to wean and
extubate early in comparison with the (SIMV)
mode with best arterial blood gases and
early discharging from the intensive care
unit.
Key words: Mode,
Weaning, Mechanical Ventilators. SIMV, ASV
|
This study
was conducted in a our busy intensive care unit
(ICU) of King Hussein medical city in the period
between November 2012 to September 2014, which
includes forty nine beds;, all our beds are occupied
most of the time. Each one is fully equipped with
standard international tools and monitors.
Most of the admitted patients are in need to be
on ventilator for different etiologies, and they
are ventilated, by using the traditional mode
already included in standard ventilators, and
watching the results of arterial blood gases for
each one in provision of early starting of weaning
and then extubation.
A new mode (which is called intelligent mode)
included in new ventilators, was optionally started
to be used in some patients. Results were analyzed
to prove the benefit of this new mode, adaptive
support ventilation ( ASV) for early weaning from
ventilator.
Most seriously ill lung patients were selected
to be on ASV mode. We start weaning of the patient
since intubated by using this mode, because the
work of breathing (WOB) is minimal and the loop
is closed; the time of ventilation was observed
to be shorter than in the other previously used
mode (SIMV). It has become a recommended way to
early extubate and then discharge of the patients
from the intensive care unit; it also a safe way
of weaning (1) which decreases the hospitalization
of patients with less use of resources, cost,
morbidity and mortality (2-6).
Adaptive support ventilation (ASV) was introduced
internationally in 1994 as an intelligent mode
of ventilation which contains the measurement
of respiratory mechanics and algorithm of closed
loop pressure control for maintaining the proper
minute volume.
After the
approval of the ethics committee of royal medical
services was obtained, one hundred and twenty
six patients were taken randomly in this study;
they were taken in two groups A and B. as shown
in Table 1.
An ordinary intubation
was done for all critically ill patients by using
Popofol or Ketamine in sleeping dose upon the
patient's blood pressure and suxamethonium chloride
in intubating dose. They were randomly assigned
to be in one of our two studied groups (A or B)
then connected to ventilator and putting the setting
reasonable for each one upon his/her condition.
Sedation was given to both groups which consisted
of two to three milligrams of morphine sulphate
as initial dose then two to three milligrams hourly
infused, and increased or decreased as needed,
for example giving either two or three milligrams
when suctioning the endotracheal tube or inserting
an intravenous line mainly in central veins. Vasopressors
or anti -hypertensive drugs were prescribed as
required for each case.
Table 1: Differences between patients and their
numbers in each group
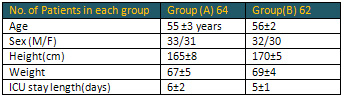
Group (A) the synchronized intermittent mandatory
volume SIMV was selected. The setting installed
is dependent on the patients' arterial blood gases,
and body weight;, seven to ten milliliter per
each kilogram body weight tidal volume (TV), fractional
inspired oxygen (FIO2), positive end expiratory
pressure (PEEP) and respiratory rate (RR) were
chosen for each case respecting the saturation
of oxygen (SPO2), metabolic state and PCO2. All
these ventilator settings were fine tuned after
obtaining the results of each arterial blood gas
(ABGs) which were taken as routine, thirty minutes
after first intubation or after attaching the
patients to ventilator. If the patient admitted
was already intubated, then ABGs were reviewed
twice daily, early morning and afternoon, or upon
any modification of the patient's condition all
through the day.
All Group B patients were attached
to ventilators by using ASV mode, which consists
of three parameters only: ideal patient's body
weight, percentage of theoretical value of minute
ventilation desired based on nomogram of Radforf
(7), and maximal inspiratory pressure tolerated
after first four to five breaths taken from ventilator.
The ventilator determines the compliance and resistance
of the patient's airways and delivers a pressure
controlled ventilation then optimizing inspiratory
pressure and respiratory rate using the formula
of Otis (8) which determines the respiratory rate
with least work of breathing as a function of
the expiratory time constant. As the patients
start to take the breath by their own effort which
is detected for each breath, the ventilator switches
to inspiratory pressure support (IPS). This level
of support is always adapted to patient's respiratory
rate and tidal volume to achieve the preset minute
ventilation using a comfortable breath pattern.
Harmful patterns like rapid shallow breathing,
high dead space ventilation, breath holding and
excessive large breath are all prevented by adjustments
of inspiratory pressure and respiratory rate which
means that the machine is continuously changing.
In both groups A and B the weaning protocol of
our ICU was applied, and the end results of each
group were analyzed by the attending intensivest
to see in which of the selected ventilator modes
(ASV versus SIMV) the early weaning and extubation
occurred.
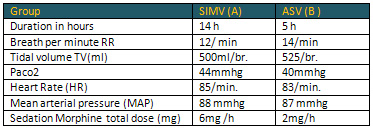
The main interesting finding
in this study was duration of weaning is shorter
in group B in comparison with group A as showed
above 5 to14 hours, intubation time also was shorter,
and then the stay length in ICU, and other parameters
like respiratory rate which was found to be little
bit lower in the ASV mode, tidal volume was found
somewhat higher in the ASV group in comparison
with the SIMV, which reflects less PaCo2 in the
ASV.
Also vital signs were taken into consideration;
the difference in both groups was watched, heart
rate (HR) and mean arterial pressure (MAP) were
shown to be minimally different in response to
different concepts of ventilation during the weaning.
Finally the total amount of sedative drugs, Morphine,
was used in significant smaller doses in the ASV
group (B), compared to the SIMV group (A); all
these findings are shown in Table 2.
Table 2: The difference in all parameters in both
groups
This study shows that using different
ventilator modes results in different variable
outcomes in the weaning process, such as time
of ventilation and then extubation which may differ
from one mode to another. In this study we compared
the most popular mode of ventilation used in the
ICUs in our region, SIMV, with the new mode called
(intelligent mode) ASV which was used in our ICU
included in the new ventilator machine
.
The great finding was observed in the group that
used the ASV mode in whom the trachea was extubated
earlier, with at least 6-24 hours than in the
other group.
In ASV group (group B) this mode provides a ventilation
in pressure support (pressure control ventilation)
and automatic change from pressure control ventilation
to inspiratory pressure support. This also leads
to fast spontaneous ventilation; the patient-machine
interaction was improved in comparison with the
SIMV mode, and this leads to early weaning from
the ventilator.
The ASV mode was possible in almost all types
patients, including the moderate respiratory failure
(PaO22/FIO2 ratio between 150-300mmhg) with appropriate
inspiratory pressure.
The smooth weaning and extubation in ASV mode
decreased the requirement of serial ABGs with
its reducing the use of resources, nursing effort,
and finally the total cost, and simplifying of
the weaning trials.
The effect of different modes on ventilator and
their safety and efficacy on patient outcomes
is difficult to assess. (9,15)
Training to use the new mechanical
ventilator modes like adaptive support ventilation
(ASV) is advisable in some patients in order to
be able to wean and extubate early in comparison
with the ( SIMV) mode with better arterial blood
gases; therefore providing early discharge from
the intensive care unit and less burden financially
and human resources.
1-Ali MJ,
Cheng DCH . Advances in cardiac Anaesthesia techniques
and intensive care. New Horiz 1999; 7:451-46.
2. Cheng DCH et al. Early tracheal extubation
after coronary artery bypass graft surgery reduces
costs and improves resource use. ANESTHESIOLOGY
1996; 85:1300-10
3. Cheng DCH et al. Morbidity outcome in early
versus conventional tracheal extubation after
coronary artery bypass grafting: A prospective
randomized controlled trial. J Thorac Cardiovasc
Surg 1996; 112:755-64
4. Silbert BS, Santamaria JD, O'Brien JL, Blyth
CM, J KW, Molnar RR. Early extubation following
coronary artery bypass surgery. Chest 1998; 113:1481-8
5. London MJ et al. Early extubation following
cardiac surgery in a veterans population. ANESTHESIOLOGY
1998; 88:1447-58
6. Cheng DCH. Impact of early tracheal extubation
on hospital discharge. J Cardiothorac Vasc Anesth
1998; 12:35-40
7. Radford EP. Ventilation
standards for use in artificial respiration. N
Engl J Med 1954; 251:877-83
8. Otis AB, Fenn
WO, Rahn H. Mechanics of breathing in man. J Appl
Physiol 1950; 2:592-607
9. Kollef MH et al.
A randomized, controlled trial of protocol directed
versus physician-directed weaning from mechanical
ventilation. Crit Care Med 1997; 25:567-74
10. Ely EW et al. Effect
of the duration of mechanical ventilation of identifying
patients capable of breathing spontaneously. N
Engl J Med 1996; 335:1864-9
11. Wood G, MacLeod
B, Moffatt S. Weaning from mechanical ventilation:
Physician-directed vs a respiratory-therapist-directed
protocol. Respir Care 1995; 40:219-24
12. Tomlinson JR, Miller KS, Lorch DG, Smith L,
Reines HD, Sahn SA. A prospective comparison of
IMV and T-piece weaning from mechanical ventilation.
Chest 1989; 96:348-52
13. Brochard L et al. Comparison of three methods
of gradual withdrawal from ventilator support
during weaning from mechanical ventilation. Am
J Respir Crit Care Med1994; 150:896-903
14. Esteban A et al. A comparison of four methods
of weaning from mechanical ventilation: Spanish
Lung Failure Collaborative Group. N Engl J Med
1995; 332:345-50
15. Morris AH. Developing and implementing computerized
protocols for standardization of clinical decisions.
Ann Intern Med 2000; 132:373-83
|