|
It must be true:
Accept your colour, stop hunting for skin whitening,
black is beautiful
......................................................................................................................................................................
Ebtisam Elghblawi
Correspondence:
Dr Ebtisam Elghblawi
MBBCh, MScRes, ADD, DRH.
Private Practice
P.O.BOX 3232
Tripoli
Libya
Email: ebtisamya@yahoo.com
|
ABSTRACT
Skin is the most voluminous structure of
the body. It not only presupposes a physiological
duty but embodies a 'social interface' among
the individual and others. It occurs to
be standing the most researchable constitution
in the cosmetic business. Generally speaking
there is an exponential interest both from
the doctors as well as our patients seeking
resolutions towards maintaining and attaining
a perfect skin.
White skin is the dream of all Arab women
with a particular attention in Libya and
a fair skin is symbolized as a beauty sign.
Libyan women tend in the summer time to
shade themselves from the sun and deprive
themselves from the benefit of sun and vitamin
D for their big wedding day. Skin lightening
cosmetics are widely used in most African
countries including Libya where Libyan women
are obsessed by it due to certain brands
ruthlessly advertising fair and lovely skin,
and it is a growing problem.
Use of cosmetic products to bleach or improve
the skin texture and colour is a habit chiefly
among dark-skinned Libyan women.
The concept of having white' skin complexion
has been considered trendy and desirable.
The active ingredients in these cosmetic
products are mainly hydroquinone, mercury
and corticosteroids in higher concentrations.
Several additives are used to enhance the
bleaching achievement.
Since these products are used mostly for
longer periods, on a large body surface
area, and under hot moist circumstances,
the per-cutaneous absorption is boosted.
Thus the complications of these products
are very detrimental and sometimes can be
deadly (Table 2).
In many instance ladies who buy those products
without any medical consultations or prescriptions
will only present to professionals when
drawbacks are incurred. Such patients have
tried everything, both at home and also
in other clinics - and on occasion spending
what amounts to a fortune on products and
treatments that have little or no effect
at all.
Hyperpigmentation disorders and skin lightening
treatments have a significant impact on
the dermatologic, physiologic, psychological,
economic, social, and cultural aspects of
life. Raising patient's awareness is vital
to avoid such irreversible complications.
To come to a close and sum up, it is mandatory
to raise more knowledge and understanding
on the occurrence and dangers of this misuse
practice.
Key words: steroids, hydroquinone,
depigmenting agents, skin bleaching, cosmetics.
|
The use of skin bleaching products
for cosmetic purposes is a very popular practice
in dark skinned women from Libya. The dermatologic
complications associated with this practice have
been comprehensively reported in the existing
literature. The aims of this review paper is
1- to shed light on the potential aspects of their
complications in the long run and to
2- enlighten about the clinical practice and the
proper advice to be given to patients who seek
such medications 3- to increase the knowledge
about the dermatological consequences of this
practice in the Libyan community.
Skin lightening (bleaching) cosmetics
and toiletries are extensively applied in most
African countries including by Libyan women in
Libya (Figures 1-3). In fact, the use of cosmetic
products to bleach or improve the skin texture
and colour is an ordinary habit among dark-skinned
Libyan women.
The usual active ingredients
in these cosmetic products are mainly hydroquinone
(strong oxidant), mercury and corticosteroids
in higher concentrations (Figures 1 & 4 &
7 & 8). Some are unknown (Figure 11). Several
additives are added to augment the bleaching effect.
Hydroquinone is a melanocyte toxic product which
combats melanogenesis (Table 1).
Table 1: different bleaching agents and mode
of action and side effects
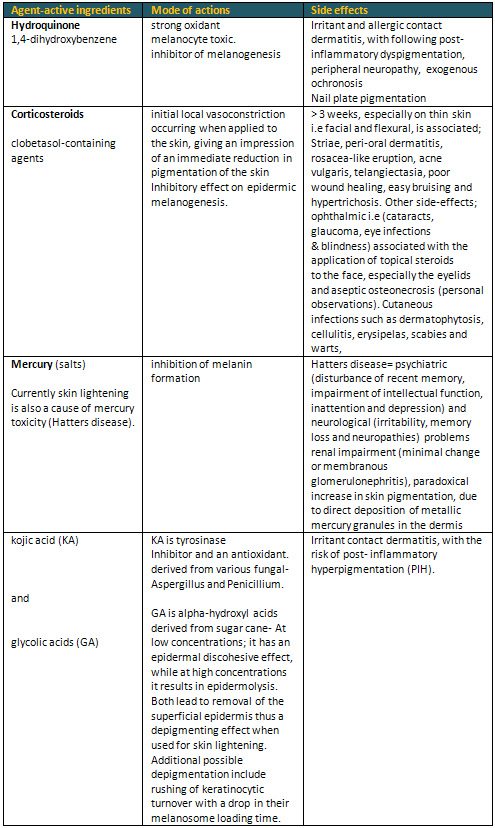
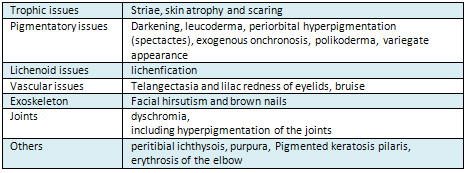
Table 2: Briefing of Aesthetic complications
Since these products are used usually for long
duration, with various concentrations, on a large
body surface area, and under hot humid conditions,
thus the per-cutaneous absorption is enhanced
and subsequently complications occur (Dadzie&
Petit 2009).
The history of practicing skin bleaching dates
back over many years in diverse communities around
the globe. In reality, in the early era around
1900s some American physicians proposed utilization
of radiation as a skin bleaching agent (Dadzie
& Petit 2009).
The complications of these
products are very detrimental and sometimes can
be deadly (Table 1). Some of the well known complications
are allergic contact dermatitis, Steroid induced
monomorphic acne (Mahé et al 2003, Nnoruka
and Okoye O 2006, Poli 2007), exogenous ochronosis
(Figure 1) (Gandhi et al 2012, Kombaté
et al, 2012), skin thinning (papering) (figure
5&6&9&10), dyschromia (Mahé
et al 2003) and hypo/hyper chromia (leucoderma)
and prominent striae atrophy (Nnoruka and Okoye
O 2006), bruise, echymosis, telangiectasias (figure
6), impaired wound healing, wound dehiscence,
with inclination to infections, candidiasis and
mycosis (Mahé et al 2003, Nnoruka and Okoye
O 2006), tinea corporis, pyoderma, cellulitis,
peri-oral dermatitis (Mahé et al 2003),
erysipelas, facial hypertrichosis and macular
hyperpigmentation of face/ macular hyperchromia
(Nnoruka and Okoye O 2006), and some claimed scabies
(Mahé et al 2003) and warts, mercurial
nephropathy, peripheral neuropathy (Mahé
and Perret 2005), cataracts, glaucoma, eye infections
and blindness, steroid addiction syndrome, immunosuppression,
lichenification, scarring, poilkiloderma, brown
nails, elastosis, roseacea, leucomelanoderma,
vibices, burn, sun burn, eczema, Diabetes mellitus
(Nnoruka and Okoye O 2006), nephrotic syndrome
(Tang et al 2013), and a broad spectrum of cutaneous
and endocrinologic complications of corticosteroids,
including suppression of hypothalamic-pituitary-adrenal
axis resulting in systemic complications such
as hypertension, hypercorticism (Pitché
et al 2005, Dadzie& Petit 2009).
In that essence, there has been a report in the
Medical Observer of Australia about a hypoadrenalism
in a 24-year-old Sudanese woman who was referred
for investigation of fertility problems and found
to have low serum cortisol (Rouse 2015). Her GP
noted she had a darker skin complexion; however
her face was a lighter shade. On questioning her
she revealed the use of two over-the-counter creams
bought at a suburban store selling African commodities;
those creams were fluocinonide 0.075% and hydrocortisone
acetate 1% and were used for many years (Rouse
2015). The explanation of the suppression of the
hypothalamic-pituitary-adrenal axis is simply
the per cutaneous steroids systemic absorption.
And in the existing literature, this has been
confirmed (Perret et al 2001). Moreover cases
of nephrotic syndrome have been reported in relation
to the use of bleaching agents where the main
culprit was mercury and such patients should be
sent for assessing the blood and urine level of
protein and mercury (Tang et al 2013).
The exogenous ochronosis is reported to occur
with higher concentration of 8% and can be seen
within 5 years of continuous application of hydroquinone
products (Ly&Soko et al 2007). However Gandhi
et al 2012 reported its occurrence with only 2%
concentrations.
Moreover hydroquinone which is composed of benzene
derivate is well known to be with carcinogenic
properties and teratogencity in vivo. Some few
studies documented the associations between developments
of cutaneous malignancy in relation to hydroquinone
(type 2). This has been claimed to be postulated
to be through its pro-carcinogenic effect or due
to suppression of the natural photo-protection
effect of melanin, however it is still a contradiction
to prove and needs further studies to confirm
(Dadzie & Petit 2009). Hydroquinone is well
known with a photosensitizing effect in different
concentrations, and has been hugely marketed for
50 years as a skin-lightening product and continues
as the most customarily used whitening constituent
in the assembly (Mahé & Perret 2005).
In the old days, hydroquinone and other cutaneous
depigmenting products were broadly prescribed
by dermatologists to combat pigmentary disorders,
and in many instances it carries a variety of
side-effects, including mercury poisoning. (Dadzie
& Petit 2009).
Issues and apprehensions have been elevated regarding
its impending dermatological and systematic side
effects, which led to ban all hydroquinone products
from the US market by the FDA on 29 August 2006
(Dadzie & Petit 2009). This has led the dermatology
community to publish some papers in regard of
this ban and address the FDA concerns and the
risks around hydroquinone. However in the third
world, including Libya, it is still considered,
prescribed and used as a lightening agent.
Wood's lamp can be a helpful tool to assess the
level of the hyperpigmentation.
Figure 1: Ochronosis

Figure 2: Uneven complexion and requested for
lightening products

Figure 3: Post strong steroids cream

Figure 4: Hyperpigmentation from different treatment
she used including strong steroids

Figure 5: Uneven colour with dark knuckle due
to strong steroids application for 4 years

Figure 6: Thin skin and telangectasia due to steroids

Figure 7: Black ladies favour this cream for whitening
- clo-betasol
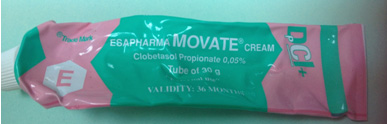
Figure 8: Patients are taken by the title WHITE
CREAM
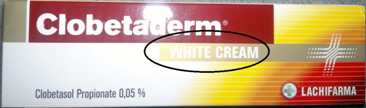
Figure 9: Post 4 years gamavate cream

Figure 10: Post 4 years gamavate cream
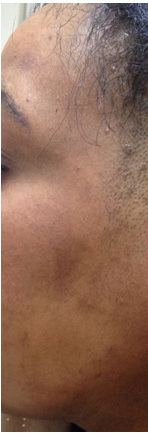
Figure 11: A cream without ingredients listed

|
LIBYAN TRADITIONAL WAYS TO LIGHTEN UP THEIR
SKIN |
The cultural practice of skin
bleaching to lighten normally dark skin
(mostly Fitzpatrick skin photo-types IV to VI)
is highly prevailing in Libya. The most common
traditional modalities of the skin bleaching practice
in Libya are: lemon, saffron and turmeric.
Some have gone far and do use different food herbs
and spices such as 2 TSF saffron or turmeric powder
with 1 TSF honey, 1 TSF rose water, 1 TSF cornstarch
and then mixing them up with 1TSF fresh lemon
juice all of which is mixed and applied on face
for one hour until it has dried up and then remove
as a scrub to lighten up their skins. Another
mix is pea's powder mixed with lemon juice in
gauze and applied as a mask on the face. Another
way is a cane milk mixed with fresh lemon juice.
Also for the body, they mix henna powder with
water and leave on the body with rose water. Also
others would mix peas with honey and rose water
and leave as a mask then peel off. Also mixing
Tafal (green material paste) or Barouuk (it's
a white stones form to grind into a white powder,
and to be mixed with rose water and applied on
the face and it is called an instant bridal whiting
complexion and well known in Tunisia) which is
mixed with rose water and left on the face until
dried up to give the whitish complexion of the
face, also dried yeast granules mixed with water
and left to ferment and then add rose water, as
well as Felyia and cucumber water mix. Also in
the old days they grind cinnamon in the mouth
and then apply on the cheeks to give the red tint.
Libyan women did not stop at this level; however
some sought the use of some creams by their peers,
to attain the whitish complexion, as some go beyond
on to using local strong steroids namely Gamavate
and Decloban creams (clo-betasol, and fluocinonide)
from OTC and I met some who think and strongly
believe they are the beauty creams. The most common
places where Libyan women tend to apply such agents
on, is face, neck, dorsa of the hands, elbows,
between thighs and knees in order. And the duration
of the practice varied from 1 month to few years
as most declared. Women tend to buy them without
any medical prescription.
The high use of super potent steroids is reported
to be alarming and striking (Mahé et al
2003). Libyan women find strong steroids application
to be appealing as they are potent lighteners
for their skin tone and complexion, and the most
observed bleaching products among black women
were the blind application of super-potent topical
steroids class I which appeared to be the main
culprits responsible for the observed skin complications
in the clinical setting.
This fact is attributed to
the easily accessibility to strong steroids which
in many instances are free of charge at polyclinics
in Libya and if not, they are available at low
prices at private pharmacies.
From my observation, it seems the most concerning
skin diseases motivating ladies visits to the
dermatology clinic are complications of that misuse
practice, i.e. pigmentation disorders or caustic
effects of their own choices of applications (Mahé
et al 2003).
In some cases the dermatological
diagnoses were based mainly on clinical grounds;
this reflects that the dermatological, where clinical
accuracy or the diagnosis of common dermatoses
appears good and perceived (Mahé et al
2003).
Also in many places where
the products claimed to be a "natural"
skin bleacher, was found to be containing higher
concentration of hydroquinone or corticosteroids,
or even both simultaneously (Mahé&
Perret 2005). I recall in the old days, ladies
were obsessed by Shirley cream and fair and lovely
cream to have a lighter skin.
Topical strong steroids have
surfaced in the latest years as chief facial skin
lighteners, due to their potent bleaching power,
and perhaps also their anti-inflammatory activity
that could limit the risks for dermatitis; nevertheless,
they appeared here as the main cause to blame
for the complications observed with ladies (Mahé
et al 2003)
Nowadays in the last few years, the new trend
is for promoting and advertising glutathione and
others as antioxidants without any harmful agents,
in the form of tablets and injections in different
strengths, and they are marketed strongly without
any proper monitoring, studies, inspection and
legislations and patients are deceived by the
description of it is magical results attained
in a few months and in most cases patients are
zealous and taking by such attractive commercials
products and are willing to pay a fortune to achieve
the ultimate wishes and yearning desire for a
fair supple skin. This is because the white and
pale skin is considered as a beauty sign and social
privileges for better groom proposal and working
chances. In Libya in many places, dark and black
skin is still considered as a negative cultural
perception and stigma. Moreover some far east
people who have olive skin, and who are more working
in the nurse field in Libya, such as Philipinos
tends to use such products more as well to attain
the white radiant skin. This phenomenon is sweeping
Europe the other way around, where western women
go to the tanning salon to acquire the dark glow.
There are many various wide varieties of different
skin-lightening brands in the Libyan market which
are being imported from overseas, and bearing
the fact of the high demand to purchase such products
for such skin- lightening products in this country
make it a flourishing business.
The total sales volume of skin lighteners is high
in Libya and there is no rough estimation due
to the lack of registrations and records.
The most common excuses for such products encountered
in the clinical settings are: to improve the skin
before marriage, to get rid of blemishes on the
face and other parts of the body, to attain a
beautiful radiant skin, to even out the skin tone
and some as a fashionable trend heard by their
peers.
Also in the clinical setting I in many instances
encountered a request for skin bleaching treatment
by some patients to lighten up their complexion.
There is not any evidence based clinical trials
yet on their safety, method of actions, nor the
long run complications and consequences. Its temporary
effects and need to be continuous as some medical
colleagues declared from their patient's outcome,
plus it is a means for a very lucrative business
for many marketing companies.
Patient awareness of their risks is vital and
thus it is critical for every practicing physician
to be aware of these complications and raise awareness
for those ladies who turn up in the clinic asking
for them officially.
Skin lightening compounds, such as hydroquinone
and topical corticosteroids, are often prescribed
and used to treat hyper-pigmentation disorders;
namely melasma, or lighten skin for cosmetic purposes.
In spite of their recognized usefulness, huge
dermatological and systematic complications have
been linked with them. Authorized bodies have
identified the drawbacks of skin lighteners and
questioned the safety of this substance, and in
fact it is nowadays forbidden in certain countries
to sell such products. This has led to the possibility
of exploring other alternatives to inhibit skin
pigmentation such as retinoids, azelaic acid,
arbutin, kojic acid, aleosin, mequinol, licorice
extract, ascorbic acid, soy proteins, and N-acetyl
glucosamine.
Dermatologists and users of such products should
be attentive of the various components in bleaching
compounds, and their potential impediments.
The management of the aesthetic complications
of artificial skin whitening causes real problems,
and the therapeutic means available are financially
inaccessible to most patients living in developing
countries. Trophic disorders, whether skin atrophy
or striae atrophicae, are beyond any therapeutic
resources.
The general state of welcoming bleaching and whiting
in the Libyan community could arise from the inherent
feeling of having a fair skin in the community
which signifies beauty and attraction to the counterpart
gender.
This article hints to a number
of traditional bleaching methods that have a certain
beauty and mystery for Libyan women's culture.
This personal observation of high demand and use
of super potent steroids is striking, as in fact
most of such products are easily accessible through
pharmacies without a prescription. The motivations
of such patients to visit a doctor are the complications
incurred of such practice.
The misuse of over-the-counter (OTC) cosmetic
and bleaching agents must be banned and forbidden
and there should be some legislation incurred
on pharmacies onto not selling such products without
a prescription, and emphasizing consulting a dermatologist
beforehand. Usually patients in Libya attain such
topical products by unregulated bodies including
pharmacies.
Such patients usually presented particularly complex
medical, social and emotional problems, where
they are desperate for a solution and willing
to pay anything.
Moreover in the dermatology communities, a discussion
on the safety of bleaching agents including hydroquinone
should offer a sole occasion to raise consciousness
and understanding about skin bleaching risks and
mandate careful consideration and selection.
Now with the introduction of the internet, some
people's access to unscrupulous suppliers via
the internet to avoid costs of professional consultation,
and most of Libyan women have an access especially
to the social media, like facebook where many
marketers use it to promote their business solo
and informally without any regulation and legislation;
they just post and ask the client privately about
the price and the delivery mode. Such marketing
places an effective tempting post, where most
women are taken in by and cannot resist, and especially
single ones and they buy them without any prior
consultation to attain that fairer skin for the
big wedding day that she ever dreamt and wished
for.
Self administration is dangerous and fraught,
not least due to no safe information about the
products name, exact formulations and safety,
neither provided nor approved by the regulatory
bodies.
The purchase of medications over the internet
is utterly poorly unregulated and this poses an
even greater problem that should be tackled and
addressed. Moreover, Libyan women can easily obtain
topical strong strength corticosteroids without
any medical prescription.
Each case reported should be taken seriously and
should be reviewed thoroughly and analyzed.
The breakdown by level of education and application
was not explored among women but most of them
state their peers applied it and advised about
it.
Aesthetic complications associated with artificial
bleaching and depigmentating products are common,
but are rarely the reason for consulting a dermatologist.
In the absence of suitable therapeutic agents,
prevention, based on informing women of the damaging
effects of artificial depigmentation, is the only
way forward.
We need to educate ladies and men's with pigmentory
problems to request early dermatological consultation
for their dermatoses, rather than to self- medicate
with over-the-counter or illegally obtained cutaneous
depigmenting bleaches to avoid complications which
would impact the patients at the sociological
and psychological levels.
There is a need for appropriate
public health prevention campaigns to raise awareness
to combat such illegal trafficking of bleaching
agents to implement.
There is a need for rigorous
scientific studies, especially in the Arab world
where such studies remain scarce, to critically
evaluate the global burden and adverse health
effects associated with skin bleaching.
In many instances, the aesthetic
complications of artificial skin bleaching causes
real problems and beyond any financial affordability,
and any possible corrections and less than optimal,
such striae atrophicae, skin atrophy, and exogenous
ochronosis. Some claimed that Nd:Yag 1064-nm laser
system is a bit effective in ochronosis.
There should be a form of protection, such as
photoprotection, should be the rule. Any product
to be used of those bleaching products must comply
with the legislation in force.
The take home message and the
general rule for such patients is to keep away
from direct sun lights, as both UVA and UVB rays
are responsible and both likewise accountable
for deepening pigmentation. For instance, UVA
rays penetrate deeper into the skin than UVB rays,
and cause wrinkles and age spots. Thus in that
instance "A" for ageing. While UVB rays
are responsible for tanning. Thus "B"
for burning. In order to combat pigmentation and
prevent further damage and protect the skin, a
sunscreen with a minimum protection of SPF30 is
mandatory and essential. Also it is vital to increase
awareness of the potential complication of cumulative
body glucocorticoid excess syndromes and the consequences
for secondary adrenal insufficiency are important
to minimise problems.
Gandhi V, Verma P, Naik G. Exogenous
ochronosis After Prolonged Use of Topical Hydroquinone
(2%) in a 50-Year-Old Indian Female. Indian Journal
of Dermatology. 2012;57(5):394-395.
Pitché P; Kombaté K; Tchangai-Walla
K, International Journal Of Dermatology [Int J
Dermatol], ISSN: 0011-9059, 2005 Oct; Vol. 44
Suppl 1, pp. 39-40
Dadzie, O. E., & Petit, A. (2009). Skin bleaching:
highlighting the misuse of cutaneous depigmenting
agents. Journal Of The European Academy Of Dermatology
And Venereology: JEADV, 23(7), 741-750
Ly F, Soko A, Ndiaye B, et al. Aesthetic problems
associated with the cosmetic use of bleaching
products. International Journal Of Dermatology
[serial online]. October 2007;46 Suppl 1:15-17
Mahé A, Ly F, Aymard G, Dangou J. Skin
diseases associated with the cosmetic use of bleaching
products in women from Dakar, Senegal. The British
Journal of Dermatology [serial online]. March
2003; 148 (3):493-500
Mahé A; Ly F; Perret JL. Systemic complications
of the cosmetic use of skin-bleaching products.
International Journal of Dermatology [Int J Dermatol],
ISSN: 0011-9059, 2005 Oct; Vol. 44 Suppl 1, pp.
37-8
Kombaté K; Mouhari-Toure A; Saka B; Akakpo
AS; Maboudou A; Pitché P; Tchangaï-Walla
K. Acne and skin bleaching in Lomé, Togo.
International Journal of Dermatology [Int J Dermatol],
ISSN: 1365-4632, 2012 Nov; Vol. 51 Suppl 1, pp.
27-9
Poli F. Acne on pigmented skin. International
Journal of Dermatology [Int J Dermatol], ISSN:
0011-9059, 2007 Oct; Vol. 46 Suppl 1, pp. 39-41
Rada Rouse. 2015. An unusual reaction to skin-lightening
cream. Medical observer. http://www.medicalobserver.com.au/medical-news/an-unusual-reaction-to-skin-lightening-cream
Perret JL, Sane M, Gning S, Ba K, Rohou G. [Hypothalamo-hypophyseal-adrenal
hypofunction caused by the use of bleaching cosmetics
in Senegal]. Bull Soc Pathol Exot. 2001;94(3):249-52
Nnoruka E, Okoye O. Topical steroid abuse: its
use as a depigmenting agent. J Natl Med Assoc.
2006; 98 (6):934-9
Tang HL, Mak YF, Chu KH, Lee W, Fung SK, Chan
TY, Tong KL. Minimal change disease caused by
exposure to mercury-containing skin lightening
cream: a report of 4 cases. Clin Nephrol. 2013;
79 (4):326-9.
|