|
Evaluation of
Epworth Sleepiness Scale as a screening method
for Obstructive Sleep Apnea Syndrome (OSAS)
......................................................................................................................................................................
Rakan M. Haddad (1)
Sultan K. AlSureehein (1)
Ghaith Abu Alsamen (1)
Majid Alzboon (2)
Abdullah Al Hazeem (2)
(1) Department of Internal Medicine, Respiratory
Medicine Division,
King Hussein Medical Center (KHMC), Amman, Jordan
(2) Department of Nursing, King Hussein Medical
Center (KHMC), Amman, Jordan
Correspondence:
Dr. R. Haddad
Department of Internal Medicine, Respiratory Medicine
Division,
King Hussein Medical Center (KHMC), Amman, Jordan
Email: Rakanhaddad@yahoo.com
|
ABSTRACT
Objective: To compare the results
of the Epworth Sleepiness Scale (ESS) score
and the Apnea-Hypopnea Index (AHI) measured
by overnight polysomnography in patients
diagnosed to have Obstructive Sleep Apnea
Syndrome in King Hussein Medical Center
(KHMC), to evaluate the Epworth Sleepiness
Scale as a screening method for OSAS.
Method: Retrospective study of patients
diagnosed to have obstructive sleep apnea
syndrome between 2013 and 2015. Epworth
Sleepiness Scale score and Apnea-Hypopnea
Index of 118 patients were compared.
Results: Of the 118 patients diagnosed
to have Obstructive Sleep Apnea Syndrome,
65 patients had a score of >10 on the
Epworth Sleepiness Scale, which translates
to 55% of the patients studied. 100% of
patients with severe OSAS had an ESS score
>10. However, in patients with moderate
and mild OSAS, 46.5% and 36% scored >10
on the ESS respectively.
Conclusion: Epworth Sleepiness Scale
is sensitive in patients with severe OSAS.
However, the accuracy of the ESS becomes
less in mild and moderate OSAS, making it
a poor and non-accurate screening method
for OSAS.
Key words: Epworth Sleepiness Scale
(ESS), Obstructive Sleep Apnoea Syndrome
(OSAS), screening
|
Obstructive Sleep Apnea Syndrome
(OSAS) is common, affecting approximately 4% of
middle-aged men and 2% of middle -aged women.
(1) However, these figures are an underestimation,
and about 95% of patients with sleep disorders
are not diagnosed.(2,3) It is very important to
diagnose and manage OSAS efficiently, because
OSAS is independently associated with increased
morbidity and mortality due to cardiovascular
and neurovascular diseases, metabolic disorders
and impaired neurocognitive function.(4,5,6)
Overnight polysomnography (PSG) is the gold standard
for diagnosing OSAS. However, the PSG is expensive,
time consuming and not widely available outside
big medical centers. Another problem is the long
waiting time for PSG. All of these issues urge
us to find a simple and reliable way to screen
patients for the probability of OSAS before referring
them to an overnight polysomnography.
Many tests have been evaluated and studied. The
Multiple Sleep Latency Test (MSLT) is believed
to provide a reliable measurement of sleepiness.
(7,8) The Maintenance of Wakefulness Test (MWT)
(9) and the Modified Assessment of Sleepiness
Test (MAST) (10) were also shown to be reliable
when it comes to evaluating patients with sleep
disturbances. However, all these tests have the
same disadvantage of being cumbersome, expensive
and time consuming.
The Epworth Sleepiness Scale was developed in
1991, and was suggested as a screening method
for patients with suspected OSAS. Despite the
fact that it is subjective, ESS has the advantage
of being fast, free and easy to be applied. (11)
Our aim in this study is to evaluate the Epworth
Sleepiness Scale (ESS) as a screening method for
OSAS.
The study was done by analyzing
the files of 118 patients who underwent overnight
polysomnography (PSG) in KHMC between 2013-2015.
They were all diagnosed to have OSAS (defined
as AHI?5 ). The pre-treatment ESS score of these
patients was compared to their Apnea-Hypopnea
Index (AHI) obtained during the PSG. An ESS score
of >10/24 is considered to be suggestive of
excessive daytime sleepiness (EDS) (12), and warrants
further evaluation by PSG to rule out OSAS.
In our study group which consisted
of 118 patients with OSAS, 47 patients had mild
OSAS (defined as AHI 5-15), 43 patients had moderate
OSAS (AHI >15-30) and 28 patients had severe
OSAS (AHI>30).
By comparing the results of the ESS score and
AHI of these patients, it was found that 65 patients
from our study group had an ESS score >10.
This represents 55% of the patients included in
the study.
All 28 patients with severe OSAS had an ESS score>10,
which means that ESS score was suggestive of EDS
in 100% of patients with severe OSAS in our study
group.
From the 43 patients diagnosed
with moderate OSAS, 20 patients had an ESS score>10,
which means that 46.5% of patients with moderate
OSAS in our study group had an ESS score suggestive
of EDS.
From the 47 patients with mild OSAS, 17 patients
had an ESS score>10. This means that 36% of
patients with mild OSAS in our study group had
an ESS score suggestive of EDS.
Table 1: The number
and percentage of patients with ESS>10 in the
mild, moderate and severe OSAS groups
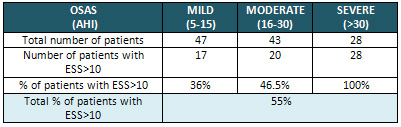
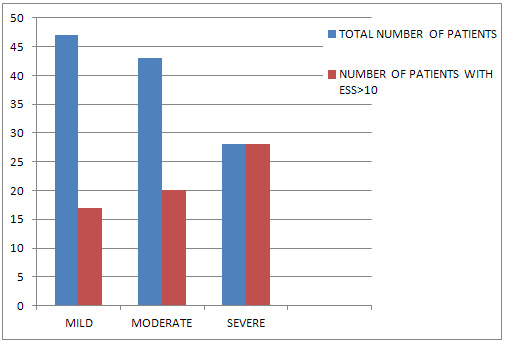
Chart 1: Comparison between total number of
patients diagnosed to have OSAS (mild, moderate
and severe) and the number of those with ESS>10
Epworth Sleepiness Scale (ESS)
was developed in 1991 by Dr. John W. Murray. It
consists of 8 questions that are supposed to evaluate
the tendency of an individual to fall asleep in
certain conditions. Each question is answered
by a number on a scale from 0 to 3 (Chart 2.)
Chart 2: Epworth Sleepiness Scale form
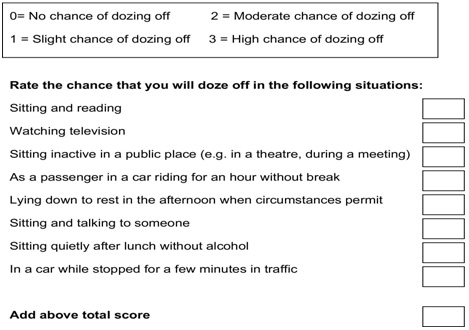
After answering all the questions in the ESS form,
a score of >10 is considered to be suggestive
of excessive daytime sleepiness (EDS), and OSAS
is highly suspected in this group of patients,
which warrants further evaluation by overnight
polysomnography. However, and according to Dr.
Murray, the evaluation by the ESS is influenced
by the patient's reading and comprehension skills
and honest answers. (11)
In our study, it was shown that the ESS is very
sensitive in patients with severe OSAS. All 28
patients with AHI>30 had an ESS score>10,
with 100% sensitivity of ESS in detecting EDS
in this group.
However, the sensitivity of the ESS gets less
when it comes to patients with mild and moderate
OSAS.
From the 47 patients diagnosed to have mild OSAS
in our study, 17 patients had an ESS score >10,
which means that only 36% of these patients had
an ESS score suggestive of EDS.
In the group of patients with moderate OSAS which
consisted of 43 patients, 20 patients had an ESS
score >10, which means that 46.5% of them had
an ESS score suggestive of EDS.
Overall, 55% of the patients who were diagnosed
to have OSAS in this study had an ESS>10, leaving
nearly half of the patients (45%) with an ESS
score NOT suggestive of EDS. This means that the
ESS has a low sensitivity as a screening method
for OSAS.
This result was also concluded by other studies,
such as the meta-analysis done by Ramachandran
and Josephs (13), which evaluated several clinical
screening tests for OSAS. They concluded that
the ESS was the least accurate of all the screening
tests examined in the study.
The ESS is a very simple, cheap
and fast way to assess patients for the possibility
of EDS and OSAS. However, it has low accuracy
in the mild and moderate OSAS groups.
Patients with mild and moderate OSAS are still
at high risk for cardiovascular and neurovascular
diseases and metabolic abnormalities, and failure
to detect these patients through screening methods
will delay their diagnosis, and thus will delay
offering them good management of their OSAS, putting
them at higher risk for complications of these
diseases. This makes the Epworth Sleepiness Scale
(ESS) not a preferable method for screening for
OSAS, and it can't be used as a sole screening
method for OSAS.
1. Young
T, Palta M, Dempsey J, et al. The occurrence of
sleep-disordered breathing among middle-aged adults.
N Engl J Med 1993;328:1230-5.
2. Bittencourt LR, Togeiro SMGP, Bagnato
MC. Diagnóstico da Síndrome da apnéia
e hipopnéia obstrutiva do sono. In: Stamm
A. ed. Rinologia; 2002; São Paulo: Komedi;
2002: 103-11.
3. Mercado JC. Identifying Obstructive Sleep Apnea:
A Highly Prevalent and Underdiagnosed Disease.
Physician Assistant 2003; 27(2): 39-45.
4. Young T, Finn L, Peppard PE, Szklo-Coxe M,
Austin D, Nieto FJ, et al. Sleep disordered breathing
and mortality: eighteen-year follow-up of the
Wisconsin sleep cohort. Sleep. 2008;31:1071-8.
5. Marshall NS, Wong KK, Liu PY, Cullen SR, Knuiman
MW, Grun Stein RR. Sleep Apnea as an independent
risk factor for all-cause mortality: the Busselton
Health Study.Sleep.2008;31:1079-85.
6. McNicholas WT, Bonsigore MR, Management Committee
of ECAB. Sleep apnoea as an independent risk factor
for cardiovascular disease: current evidence,
basic mechanisms and research priorities. Eur
Respir J. 2007;29:156-78
7. Richardson G, Carskadon M, Flagg W, Van Den
Hoed J, Dement W, Mitler M. Excessive daytime
sleepiness in man: multiple sleep latency measurements
in narcoleptic vs. control subjects. Electroencephalogr
Clin NeurophysioI1978;45:621-7.
8. Carskadon MA, Dement WC. The multiple sleep
latency test: what does it measure? Sleep 1985;5:S67-72.
9. Mitler M, Gujavarty KS, Browman CP. Maintenance
of wakefulness test: a polysomnographic technique
for evaluating treatment in patients with excessive
somnolence. Electroencephalogr Clin Neurophysiol1982;
153:658-61.
10. Erman MK, Beckham B, Gardner DA, Roffwarg
HP. The modified assessment of sleepiness test
(MAST). Sleep Res 1987; 16: 550
11. Murray JW. Daytime Sleepiness, Snoring and
Obstructive Sleep Apnea: The Epworth Sleepiness
Scale. Chest 1993; 103(1): 30-6.
12. Johns MW. A new method for measuring daytime
sleepiness: the Epworth sleepiness scale. Sleep
1991;14:540-5
13. Ramachandran SK, Josephs LA. A meta-analysis
of clinical screening tests for obstructive sleep
apnea. Anesthesiology. 2009;110:928-39.
|