|
Pregnancies Complicated
by Severe Autoimmune Thrombocytopenic Purpura
......................................................................................................................................................................
Amer Gharaibeh (1)
Tareq Irtaimeh (2)
(1) Amer Gharaibeh, MD, Maternal Medicine Clinic,
King Hussein Medical Center, Amman, Jordan
(2) Tareq Irtaimeh, MD, Department of Obstetrics
and Gynecology,
King Hussein Medical Center, Amman, Jordan
Correspondence:
Amer Gharaibeh, MD, Maternal Medicine Clinic,
King Hussein Medical Center, Amman, Jordan
Email: agharaibeh@hotmail.com
|
ABSTRACT
Objectives: To assess pregnancy course
and perinatal bleeding in women with severe
autoimmune thrombocytopenic purpura.
Material and methods: We collected
data of 38 pregnancies in 24 women, who
were on treatment for autoimmune thrombocytopenic
purpura early in pregnancy. Indication for
treatment was platelets count 50.000/mm3
or less. We looked for premature rupture
of membranes, premature delivery, intrauterine
growth restriction and significant blood
loss at delivery. Those women were the study
group, (group 1). The same variables were
looked for in 100 healthy pregnancies taken
as control (group 2). Data was compared
between the two groups. Information was
obtained prospectively from the woman's
follow up visits at maternal medicine clinic,
King Hussein Medical Center as well as data
gathered from women with previous pregnancies
complicated by autoimmune thrombocytopenia.
Women who had thrombocytopenia secondary
to other conditions such as systemic lupus,
bone marrow diseases and other causes, were
not included in the study.
Results: The study group 1 had nine
premature ruptures of membranes in 38 pregnancies,
whereas only ten women ruptured their membranes
out of 100 in control group 2 with an odds
ratio 2.9. Four women had significant blood
loss at delivery in group 1 and eight women
in group 2 which presents marginal increase
for group 1 (odds ratio 1.3). No increase
in growth restricted babies nor in premature
delivery was noticed.
Conclusion: Pregnant women with autoimmune
thrombocytopenic purpura on treatment, have
significant higher risk to rupture their
membranes prematurely. No increase in growth
restricted babies and premature deliveries.
With good care they can deliver safely with
minimum hazard of bleeding.
Key words: pregnancy,
complication, thrombocytopenia, bleeding
|
Pregnant women with thrombocytopenia
are not infrequently met at antenatal clinics
(7-10%)(1). Some of them are accidentally discovered
during routine blood test. Pregnancy induced thrombocytopenia
is the most encountered cause related to pregnancy(2),
whereas Idiopathic thrombocytopenic purpura is
the most encountered cause that is unrelated to
pregnancy(3). Platelets count was found normally
lower in pregnancy and decreases as pregnancy
advances(4). In one study(5), back in 2001, it
was found that platelets function in women with
pregnancy induced thrombocytopenia was preserved.
A recent study(6) emphasized on the increase in
platelets aggregation in pregnant women when compared
to non-pregnancy state. Pregnancy course and the
complications that may be encountered are attributed
to the disease itself or to drugs used to ameliorate
the disease. Studies are conducted to minimize
the risk of thrombocytopenia on pregnant women
and on the developing fetus. Management needs
to balance between the hazard of low platelets
count and the risk of drugs used on the mother
and the fetus. When medication is needed, corticosteroids
are first line of treatment(7). It is known for
its side effect on blood pressure, glucose tolerance
and immunity among others(8). Other immunomodulating
drugs are used which are not risk free.
It may be difficult to distinguish between gestational
induced thrombocytopenia and ATP when first recognized
during pregnancy(9), nevertheless, gestation induced
thrombocytopenia is known to have mild disease
course. Actual platelets count has to be looked
for sometimes when platelets clumps are formed.
Tubes with different anticoagulant media are used.
Sodium citrate, heparin Ethylenediaminetetraacetic
acid tubes are dispatched to the lab, platelets
count can be performed manually when suspicion
of clumping or agglutination arises(10).
The aim of our study is
to look for pregnancy course in women with severe
autoimmune thrombocytopenia, in regard to premature
rupture of membranes, to fetal body weight at
delivery, prematurity and peripartum bleeding.
In our study we followed
the course of pregnancies complicated by severe
autoimmune thrombocytopenia, which were diagnosed
prior to pregnancy, or first discovered during
gestation. Severe thrombocytopenia is when platelets
count decreases to less than 50,000 x 109/L(11).
24 pregnant women with 38 pregnancies
diagnosed with severe autoimmune thrombocytopenic
purpura were considered in the study; they were
taken as study group and labeled as (group one).
Another 100 women with normal course pregnancy
and normal platelets count were also included
in the study as control group and labeled as (group
two). Severe thrombocytopenia is when platelets
count decreases to less than 50,000/mm3. They
were followed up at maternal medicine clinic,
Obstetrics department. Data were obtained prospectively
from patients' follow up records and retrospectively
of previous pregnancy and post natal visits. All
women were on oral steroids; some of them had
other immune modulating drugs added. An oral steroid
(Prednisolone) was use in a dose of 20 to 60 mg.
Azathioprine in doses 50 to 100 mg was added in
4 women. Two women received intravenous immunoglobulin
for resistant disease at gestational age 28 for
one of them and at 30 weeks for the second patient.
The aim of treatment was to keep platelets count
at or above 40.000/mm3. Citrate, heparin or ethylene
diamine tetra acetic acid tubes were dispatched
to the laboratory. Manual count was also requested
when suspicion arises. No considerable spontaneous
bleeding was met and thus no blood transfusion
was considered for any patient before delivery.
Minor epistaxis resolved by local hemostatic care.
Platelets transfusion was considered only at delivery
or before surgery to raise platelets count up
to 50.000/mm3.
The course of pregnancy and bleeding at delivery
was studied and compared between the two groups.
We looked at premature rupture of membranes, premature
delivery, babies small for gestation age and amount
of blood loss at delivery.
Premature rupture of membranes was defined as
amniotic fluid passage before onset of labour
at any gestational age. Deliveries before 37 weeks
completed of gestation were taken as premature
delivery. Fetal body weight at delivery at or
less than the 10th centile was considered small
for gestational age. Blood loss was considered
significant when hemoglobin concentration decreases
by 2gr/dl or more for vaginal delivery and 3gr/dl
or more after operative delivery. Caesarean section
was conducted for obstetric reasons or as maternal
request after counseling the family.
Using MedCalc software, Odds ratio and confidential
intervals and p-value were calculated.
38 pregnancies with severe thrombocytopenia
were included in the study, all of them were on
oral Prednisolone 20 mg and up to 60 mg. Azathioprine
was added in a dose of 50 up to 100 mg for 4 women
who were resistant to Prednisolone alone. Two
cases did not respond to Prednisolone and Azathioprine;
they received Intravenous immunoglobulin and 8
women needed platelets transfusion when in labour
or before operative delivery.
Nine women in study group ruptured their membranes
before the onset of labour (23.6%), four had significant
bleeding (10%), five delivered babies at or below
the 10th centile (13%), and four had premature
deliveries before 37 weeks completed (10%).
In the control group the results were 10 (10%),
8(8%), 12(12%), 11(11%) respectively, (Table 1).
Table 1: Comparison in pregnancy course and
peripartum bleeding between groups
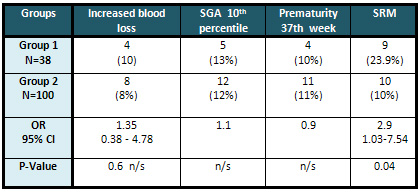
n/s= not significant
Spontaneous rupture of membranes was significantly
increased in women with severe thrombocytopenia
on treatment than in women with no steroid treatment
and normal platelets with an odds ratio of 2.9,
(95% CI 1.03-7.53).
There was minimal increase in peripartum bleeding,
(OR 1.3, 95% CI 0.3-4.7); it was not statistically
significant. No blood replacement was needed.
No difference was found in the rates of premature
deliveries or in small for gestation babies between
the two groups.
Women with thrombocytopenia
present a special challenge to obstetricians in
the fertility period. Bleeding that may occur
during pregnancy and delivery due to obstetric
reasons has particular hazard when thrombocytopenia
is superimposed. The Obstetrician has to place
platelet count at safe levels to ensure maternal
health. Drugs used in the aim of achieving this
goal may not be risk free. In our study we tried
to estimate the hazard of medication used in managing
thrombocytopenia in pregnancy.
Prednisolone, a synthetic corticosteroid is the
first line and main stay treatment. It was found
not to cause major fetal abnormalities (12,13)
. Nevertheless the risk of premature rupture of
membranes has been recognized by different studies(14).
In accordance with those studies, we found that
premature rupture of membranes occurred more frequent
in thrombocytopenic women on Prednisolone. It
is difficult to establish if the increase in premature
rupture of membranes is exclusively due to steroids
treatment or thrombocytopenia per se presents
an independent risk factor.
Blood loss at delivery was marginally increased
in women with thrombocytopenia. This emphasises
the fact that platelets function is preserved,
and the hazard of peripartum bleeding is not immense,
particularly when appropriately managed.
Excluding cases with premature rupture of membranes,
premature delivery was not increased in our study.
This leads to the conclusion that thrombocytopenia
is not a direct risk factor for premature delivery.
The risk of small for gestation babies at delivery
was not increased also. This highlights the normal
fetal growth pattern, normal oxygenation and nutrition.
Our results suggest that pregnant
women with severe autoimmune thrombocytopenia
on treatment have an increased risk to rupture
their membranes prematurely. This may be due to
medications used in managing the condition, or
due to the disease itself. Risk of bleeding may
exist, but with appropriate care and management
it is of low risk. Fetal growth and premature
deliveries are not more likely in isolation of
premature rupture of membranes.
Number of subjects represented a limitation to
the study; more studies in larger numbers are
needed to verify those results.
1. Myers B. Diagnosis and management
of maternal thrombocytopenia in pregnancy. Br
J Haematol. 2012;158(1):3-15.
2. Gernsheimer T. Thrombocytopenia in pregnancy:
is this immune thrombocytopenia or …? Hematology
Am Soc Hematol Educ Program. 2012;198-202.
3. Gernsheimer T, James A, Stasi R, How I treat
thrombocytopenia in pregnancy. Blood. 2013;121(1):38-47.
4. Nisha S, Amita D, Uma S, Tripathi AK, Pushplata
S. Prevalence and characterization of thrombocytopenia
in pregnancy in Indian women. Indian J Hematol
Blood Transfus. 2012;28(2):77-81.
5. Vincelot A, Nathan N, collet D, Mehaddi Y,
Grandchamp P and Julia A. Platelet function during
pregnancy: an evaluation using the PFA?100 analyser.
Br.J.Anaesth. 2001; 87(6): 890-893.
6. Burke N, Flood K, Muellers S, Murray A, Dempsey
M, Geary M et al. An overview of platelet function
in normal and complicated pregnancies. Expert
Review of Obstetrics & Gynecology 2013; 8:4,
379-386.
7. Bhoria P, Sharma S, Varma N, Malhotra P, Varma
S, Luthra M. Effect of steroids on the activation
status of platelets in patients with Immune thrombocytopenia
(ITP). Platelets. 2015;26(2):119-26.
8. Liu D, Ahmet A, Ward L, Krishnamoorthy P, Mandelcorn
E , Leigh R, Brown J, Cohen A, Kim H. A practical
guide to the monitoring and management of the
complications of systemic corticosteroid therapy.
Allergy Asthma Clin Immunol. 2013; 9(1): 30.
9. Boehlen F. Thrombocytopenia during pregnancy.
Importance, diagnosis and management. Hamostaseologie.
2006;26(1):72-4; quiz 75-8.
10. Kumar T, Bhardwaj N. Platelet cold agglutinins
and thrombocytopenia: A diagnostic dilemma in
the intensive care unit. Journal of anesthesiology
and clinical pharmacology. 2014; 30 (1): 89-90.
11. Erkurta A., Kayaa E., Berbera I., Koroglua
M., Kukua I. Thrombocytopenia in Adults: Review
Article. J Hematol. 2012;1(2-3) 44-53.
12. Park L, Mazzotta P, Pastuszak A, Moretti M,
Beique L, Hunnisett L et al. Birth defects after
maternal exposure to corticosteroids: prospective
cohort study and meta-analysis of epidemiological
studies. Teratology 2000 62: 385-392.
13. Hviid A, Molgaard D. Corticosteroid use during
pregnancy and risk of orofacial clefts. CMAJ.
2011;19;183(7):796-804.
14. Jain V, Gordon C. Managing pregnancy in inflammatory
rheumatological diseases, Review article .Arthritis
Research & Therapy 2011, 13:206.
|