|
Imaging of antrochoanal
polyposis
......................................................................................................................................................................
Sufian A. Al Roud
(1)
Mohammad I. Al Rawashdeh (1)
Bdewi M. Awamleh (2)
(1) Department of ENT Royal
Medical Services (RMS)
King Hussein Medical Centre
Amman, Jordan.
(2) Department of Radiology, King Hussein Medical
Centre
King Hussein Medical Centre
Amman, Jordan
Correspondence:
Dr Sufian Al Roud
Amman, Jordan
Tel: 0777745292
Email: sufian.roud@yahoo.com
|
ABSTRACT
Objective :
The aim of this study was to evaluate the
common radiological features in initial
and post operative follow up imaging of
patients proved to have antrochoanal polyposis,
and who were treated surgically, and to
evaluate post operative clinical improvement
of this sample.
Methods : A total
number of 54 patients ages between 12 and
46 years, with mean age of 21.3 years, who
proved to have ACP investigated by CT-Scan
during a 3 year period (between May 2009
and February 2012) were retrospectively
evaluated and follow up imaging CT-Scan
was performed for this group of patients.
The main presenting clinical symptom of
the selected patients was nasal obstruction.
We selected a coronal sinus CT-Scan as referral
imaging modality for this study and according
to which we made our calculations and conclusions.
Results : Unilateral
polyposis was found in 38 patients (70.4%)
and bilateral in 16 patients ( 29.6%). All
patients were operated on by Functional
Endoscopic Sinus Surgery (FESS). The patients
were followed up by CT-Scan axial and coronal
views at 4-6 weeks post operatively and
only in 7 patients we recorded a post operative
inflammatory finding of which in 2 patients
the diagnosis was recurrent antrochoanal
polyp.
Conclusion :
We conclude that CT-Scan was very accurate
in diagnosing antrochoanal polyp in pre
and post operative assessment and the recurrence
of this disease was very minimal according
to follow up clinical and imaging results.
The Functional Endoscopic Sinus Surgery
(FESS) was very effective in preservation
of normal antral mucosa with minimal complications
in post operative follow up.
Key words: Antrochoanal polyposis,
CAT-Scan, FESS
|
Antrochoanal polyposis(ACP) is
not uncommonly found in the general population
investigated for paranasal sinus pathology; it
represents a herniated maxillary sinus polyp through
the ostium reaching the nasopharynx in the majority
of cases and accounts for about 3-6% of all paranasal
polyps. Imaging of these patients plays an essential
part in managing and follow up of surgical treatments.
The prevalence of this pathology is more prominent
in pediatric and young adult age groups.
Killian was the first to describe choanal polyp
(CP) in 1906 and considered it as a large solitary
polyp originating from maxillary sinus mucosa
and redirected posteriorly reaching the nasopharynx.
This process takes part through the accessory
ostium of the maxillary sinus(1). Many recent
studies prove that not only is the accessory ostium
the solitary anatomical origin of this medical
entity, but it can also originate from sphenoid
sinus and sphenoethmoidal recess and rare cases
have been reported from the frontal sinus. This
clarification was approached by the newly developed
imaging modality machines, such as helical computerized
tomography machines CAT-Scan and MRI . These pear
shaped form antrochoanal polyps are seen usually
solitary and unilateral in the majority of cases,
differentiating them microscopically from common
nasal cystic polyps(2).
The presenting features are common in children
and young adult age groups(3) . ACP recurrence
after surgical removal is not uncommon in many
studies being reported in literature(4). These
lesions are usually benign and cause no bony or
cartilaginous destructive changes of the maxillary
boundaries, but can enlarge and extend in all
directions. The commonest is the nasopharynx causing
postnasal air route obliteration(5). Nowadays
appropriate diagnosis is made by nasal endoscopy
and computed tomography in axial and coronal views
so as to make a final management plan for each
case, considering that definite treatment is surgical
in all cases(6). With improving new modalities
of imaging machines, such as helical CAT Scans
in multiplanar reformats, the diagnosis of these
lesions is becoming more accurate excluding bony
and dental artifacts(7).
A total number of fifty four
patients, aged between 12 and 46 years, with mean
age of 21.3 years, were retrospectively analyzed
and investigated by CT-Scan (Mx 8000 Dual helical
Philips) during a three year period (between May
2009 and February 2012). The main presenting clinical
symptom of each patient was nasal obstruction.
Axial and coronal CT-Scan in multiplanar reformat
for the paranasal sinuses was performed for all
these all patients and a follow up postoperatively
according to clinical request was done. We selected
coronal sinus CT-Scan as referral imaging modality
for this study and according to which we made
our calculations and conclusions.
Among patients included in this
study (Table 1), unilateral antrochoanal polyps
were found in 38 patients(70.4%) and bilateral
in 16 patients (29.6%). All patients were operated
on by Functional Endoscopic Sinus Surgery (FESS).
All patients were followed up 4-6 weeks post operatively
and only in 7 patients we recorded a post operative
inflammatory finding of which in two patients
the diagnosis was recurrent antrochoanal polyp
(Figure 3).
Table 1: Frequency of unilateral antrochoanal
polyps and recurrence of post operative percentages
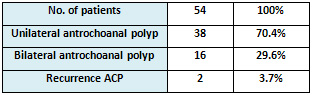
Figure 1: axial (a) & coronal (b) CT-Scan
of 21 years old male patient showed huge lobulated
right antrochoanal polyp filling right nasal cavity
and post-nasal space.
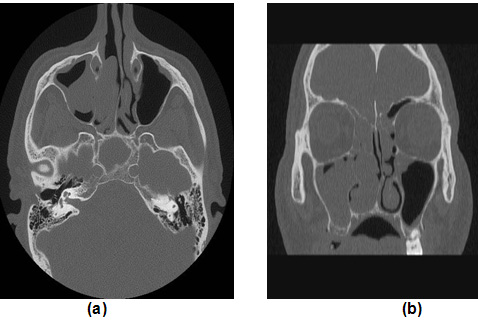
Figure 2: Well defined soft tissue density polypoidal
lesion arising from Right maxilla and extending
posteriorly into nasopharynx of a 15 year old
female patient. Note the complete blockage of
Right Choana.
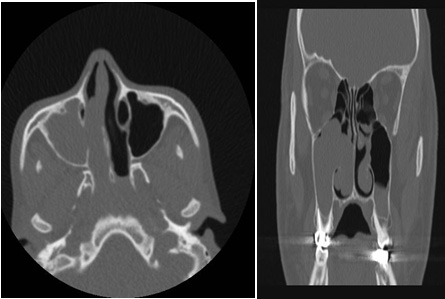
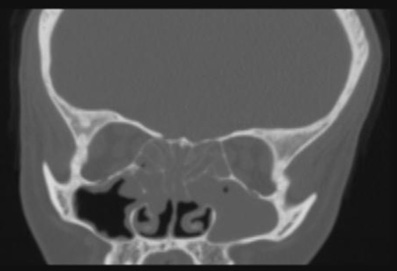
Figure 3: Inflammatory process and polypoidal
lesion in left maxillary antrum with opacification
of nasal cavity and ethmoidal sinuses in a 13
years old boy who underwent polypodectomy three
months before. The lesion represents a recurrent
polyp.
Unilateral benign paranasal
polyp represents a disease that affects the child
age group as well as young adults with no preferences
regarding the sex preponderance, and in a few
recent studies male patients are slightly more
frequently seen (8). The etiology of this disease
is mentioned as uncertain, but many theories describe
the previous inflammatory processes and allergy
that affect the mucosal layers of the sinus as
a predisposing factor which remain unproved for
other groups of editors(9). Antrochoanal polyp
usually arises from mucosal lining maxillary sinus
in the majority of cases and extends posteriorly
through an accessory ostium into the nasal cavity
which can be enlarged to obliterate the choanal
and nasopharynx. The patient is usually young
adult who complains of unilateral nasal obstruction
worsening on expiration. When the disease progresses,
this can block the Eustachian tube. Many diagnostic
modalities are implicated in supporting a management
plan for ENT surgery physicians, nasal endoscopy,
computerized tomography (CT-Scan) and magnetic
resonance imaging (MRI) are considered the main
investigations used to detect uni- or bilateral
nasal polyposis. When CT-Scan is used, the diagnosis
is made by detecting a mass which fills the maxillary
antrum and which goes through the accessory or
original ostium into the choana [Figure 1&2].
MRI shows T1 hypointense and T2 hyperintense lesions
within the antrochoanal regions (10). In our study
we used just CT-Scan as the diagnostic modality
of choice for all patients; the axial and coronal
reformats were the preferred methods of choice.
Differential diagnosis was made with other nasopharyngeal
masses, including juvenile nasopharyngeal angiofibroma,
meningioencephalocele, nasal glioma, hemangioma,
adenoids and nasopharyngeal malignancy as well
as lymphoma(11). A proper history and vigorous
clinical evaluation along with careful selection
of investigatory methods all were helpful in differentiating
antrochoanal polyp from other suspected lesions.
The frequent differential diagnosis was done with
Juvenile nasopharyngeal angiofibroma due to similarity
of presentations and almost affecting the same
age groups of patients, which is usually highly
vascular benign neoplasm with potential for local
destruction, and it is commonly associated with
epistaxis(12-14). Surgical removal was the method
of choice in treating our patients and the Functional
Endoscopic Sinus Surgery ( FESS) was done for
each patient. Complications were seen in a minority
of patients which correlates well with other studies
and did not exceed 4% of all cases, which is in
the range of many international centers (15-17).
We conclude that CT-Scan in axial
and coronal views was sufficiently accurate in
diagnosing antrochoanal polyp in pre and post
operative assessment and the diagnostic nasal
endoscopy remains in limited use. Recurrence of
this disese was very minimal according to follow
up clinical and imaging results. The Functional
Endoscopic Sinus Surgery (FESS) was very effective
in preservation of normal antral mucosa with minimal
complications in post operative follow up screening.
1. Andrey
Loatin, Valentina Bykova, Gennady Piskunov.Choanal
polyps: One entity, one surgical approach? Rhinology,35,79-83,1979.
2. BHAT M, VAIDYANATHAN V .Sausage In The Throat.
A Case Of Giant Antrochoanal Polyp. Journal of
Clinical and Diagnostic Research, 2010 April,(4):2281-2285.
3. Kiminori Sato, MD, PhD; Tadashi Nakashima,
MD. Endoscopic Sinus Surgery for Chronic Sinusitis
with Antrochoanal Polyp. Laryngoscope 110: September
2000.
4. P.FROSINI, G.PICARELLA, E.DE CAMPORA. Antrochoanal
polyp: analysis of 200 cases. ACTA OTORHINOLARYNGOLOGICA
ITALICA 2009;29:21-26.
5. Richard TOWBIN, J.S DUNBAR, KEVIN BOVE. Antrochoanal
polyps. AMERICAN ROENTGEN RAY SOCIETY, AJR 132:27-31,JANUARY
1979.
6. Huseyin Yaman et al. Evaluation and Management
of Antrochoanal Polyps. Clinical and Experimental
Otorhinolaryngology Vol. 3, No. 2: 110-114, June
2010.
7. Kate O .Connor et al. Sinus Imaging. Auckland
Radiology Group June 2010.
8. David Viros Porcunav et al. Unilateral Benign
Choanal Polyp: Review of 51 Patients.Acta Otorrinolaringol
Esp.2008:59(2):52-6.
9. E.A.CETINKAYA. Giant antrochoanal polyp in
an elderly patient. Acta Otorhinolaringol ital
2008,28:147-149.
10. Miguel Maldonado et al. The antrochoanal polyp.
Rhinology, 43, 178-182, 2004.
11. Leyla Kansu, Erdinç Aydin. Atypical
presentation of antrochoanal polyp in a child.
The Turkish Journal Of Pediatrics 2011,53,320-324
12. Mehmet Fatih Garça, Sevil Ari Yuca,
Köksal Yuca. Juvenile Nasopharyngeal Angiofibroma.
European Journal Of General Medicine.
Eur J Gen Med 2010,7(4),419-425.
13. Trevor Hackman et al. Juvenile nasopharyngeal
angiofibroma: The expanded endonasal approach.
American Journal of Rhinology &Allergy.
January-february 2009,vol.23,no 1.
14. Metin nerci,Oguz gretmenoglu, Taskin Yücel.
Juvenile nasopharyngeal angiofibroma: a revised
staging system. Rhinology, 44, 39-45, 2006.
15. Abdulrahman Al Sanosi. Endoscopic Excision
of the Antrochoanal Polyp. Kuwait Medical Journal
2005, 37 (3): 182-184 .
16. Soon Kwan Hong, Yang-Gi Min, Chong Nahm Kim,
Sung Wan Byun. Endoscopic Removal of the Antral
Portion of Antrochoanal Polyp by Powered Instrumentation.
Laryngoscope 111: October 2001.
17. Ta-Jen Lee, and Shiang-Fu
Huang, Taipei, Taiwan. Endoscopic sinus surgery
for antrochoanal polyps in children. Otolaryngology-Head
and Neck Surgery (2006) 135, 688-692
|